Digestive System
We will study the digestive system. It has time bound motility as well as secretions, responsible for processing the food. This system is meant for processing the food we eat. It is transformed into carbohydrates, proteins, fats and vitamins which provide energy to our body.
Gastrointestinal tract is a long tube starting from esophagus. It has 4 layers. From deeper to superficial layers, there are mucosa, submucosa, muscularis and serosa. (Fig. 1)
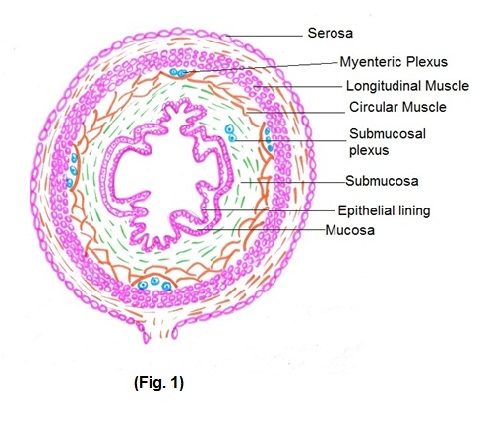
- Mucosa – This layer comes in direct contact with food. It is made up of 3 layers out of which Epithelium covers the mucosa. Mucosa is responsible for digestive, absorptive and secretory processes.
- Submucosa – It consists of dense irregular connective tissue with large blood vessels, lymphatic vessels and submucosal plexus wherein autonomic nerve fibers are interspersed with ganglion cells.
- Muscularis – It consists of smooth muscles, formed by inner circular muscle and outer longitudinal muscle fibers. Involuntary contractions of these muscles help in mixing food with digestive juices secreted by liver and pancreas and propulsion of it along the tract.
- Serosa – It is a serous membrane consisting of areolar connective tissue.
Digestive system (Fig. 2) is composed of two groups of organs
i) gastro-intestinal tract and ii) accessory digestive system.
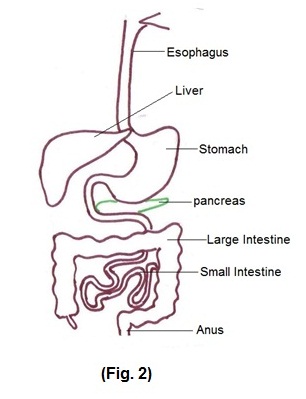
Gastrointestinal tract extends from mouth to the anus. Food enters into the esophagus through mouth and pharynx. There is upper esophageal sphincter at the level of pharynx, which opens only during swallowing. There is lower esophageal sphincter at the junction of esophagus and stomach, through which food enters into stomach. Stomach has three parts — fundus, body and pylorus. From stomach food enters into small intestine which is connected to stomach through the pyloric sphincter. Small intestine is divided into duodenum, jejunum and ileum. From ileum food enters into the large intestine through ileo-cecal sphincter. The parts of large intestine are cecum, colon, rectum and anal canal. Sphincters are orifices surrounded by muscles to store the contents for a specific period of time.
Now, we will see the control of digestive system. It includes enteric nervous system, autonomic nervous system and hormonal control.
a) Enteric nervous system – It is also called as brain of the gut. Neurons of enteric nervous system are arranged into two plexuses.
- Myenteric plexus — The motor neurons of this plexus supply smooth muscles. Thus, it mainly controls gastrointestinal motility.
- Submucosal plexus — It lies in submucosa and controls secretions of the organs of gastrointestinal tract.
b) Autonomic nervous system – Vagus nerve supplied by parasympathetic fibers mainly increases gastrointestinal secretions and motility of gastrointestinal tract. Sympathetic nerve that supply gastrointestinal tract mostly inhibit secretions and motility of gastrointestinal tract.
c) Hormonal control – Various hormones like gastrin, cholecystokinin, secretin control gastrointestinal tract secretions. e.g. Gastrin stimulate gastric acid secretions.
Functional aspects of digestive system:
A person eats food when he is hungry. Sensation of hunger arises because of stimulation of hunger center in hypothalamus. When we see, smell and even think of food the messages from cerebral cortex are sent to hunger center. Similarly, there are various factors responsible for stimulation of satiety center which prevents a person from overeating. e.g.
- Gastrointestinal tract filling — When stomach and duodenum become distended, stretch inhibitor signals are transmitted through vagus to stimulate satiety center.
- Cholecystokinin (CCK) hormone is released in response to fat and protein entering the duodenum, sending messages to satiety center via vagus nerve.
Long term regulation of hunger —
Decrease in blood sugar and exposure to cold weather stimulates hunger center. While increase in blood sugar and adipose tissue and exposure to hot weather causes stimulation of satiety center. Even before eating, salivation and gastric juice secretion starts by sight, smell and thought of food due to parasympathetic stimulation. Main function of saliva is to keep mucus membrane of the mouth moist. Chewing helps in mixing food bolus.
Next step is swallowing. It has 3 stages.
- Voluntary stage of swallowing – From mouth, food goes into pharynx due to movements of tongue.
- Pharyngeal stage of swallowing – As the bolus enters pharynx, it stimulates swallowing receptor area around pharynx, which in turn sends signals to brain stem to initiate pharyngeal muscles contraction. These contractions of pharynx propel the food by peristalsis into esophagus. There are series of automatic pharyngeal muscles contraction as follows —
- The soft palate is pulled upward to close posterior nares to prevent reflux of food into nasal cavities.
- Larynx and pharynx are elevated, larynx gets closed by epiglottis.
- Upward movement of larynx also pulls up and enlarges the opening of esophagus. At the same time upper esophageal sphincter relaxes and food enters into esophagus.
- Esophageal stage of swallowing — The esophagus functions primarily to conduct food rapidly from pharynx to the stomach. This is achieved by peristaltic movements which are responsible for relaxation of lower esophageal sphincter. If lower esophageal sphincter fails to close adequately, stomach contents can reflux into esophagus leading to gastro-esophageal reflux disease (GERD).
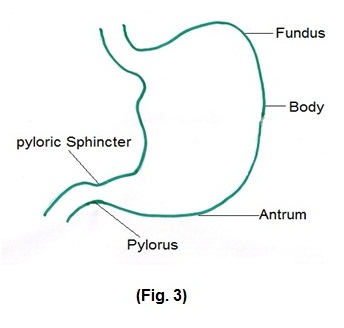
Stomach (Fig. 3)
In the stomach, stretch reflexes get activated by food and parasympathetic stimulation
results into secretions of acetylcholine, histamine and gastrin, which in turn stimulate and regulate gastric juice in stomach. Several minutes after food enters into the stomach, gentle peristaltic movements and mixing waves pass over the stomach. These waves macerate food, mix it with gastric juice, reduce it to soupy liquid called as chyme. As food reaches the pylorus, mixing and peristaltic waves become strong which force the food into duodenum. This emptying of stomach is regulated by degree of constriction of pyloric sphincter, which is increased or decreased through nervous and hormonal control. It occurs within 2 to 4 hours after eating meal. Stomach emptying is inhibited by entero-gastric reflexes from duodenal wall which depend on distension of duodenum and degree of acidity of food and hormone cholecystokinin from duodenum.
Small intestine
When portion of small intestine gets distended with chyme, it causes mixing contractions which helps mixing of food with secretions of small intestine.
Secretions of small intestine are —
- Pancreatic juice — It is secreted most abundantly in response to presence of chyme in the upper portion of small intestine which helps in digestion of proteins, fats and carbohydrates. When food enters the small intestine, Acetylcholine released from the parasympathetic vagus nerve endings in enteric nervous system. At the same time Cholecystokinin is secreted by duodenal and upper jejunal mucosa. Cholecystokinin and Acetylcholine both stimulate pancreas resulting in production of large quantity of pancreatic enzymes.
- Secretin — It is secreted by the duodenal and jejunal mucosa when highly acidic food enters into small intestine. Main function of it is to neutralize acidic chyme.
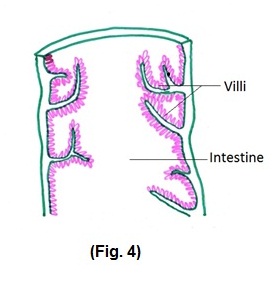
- Bile salts – Gall bladder empties its store of concentrated bile into the duodenum. Bile salts play an important role in fat digestion and absorption. Bile also serves as a means for excretion of several important waste products from blood. Wall of the small intestine has crypts and villi as shown in the (Fig 4). Crypts secrete digestive enzymes which help in digestion of fats and carbohydrate in small intestine.
Large intestine
Unlike small intestine there are no villi in large intestine. Epithelial cells of large intestine secrete large amount of mucus when food enters into it by local nervous reflexes to the mucous cells. Stimulation of pelvic nerves from the spinal cord, which carry parasympathetic innervations to large intestine, also causes mucus secretion.
When large intestine is irritated by any foreign particle, mucosa of large intestine secretes extremely large quantity of water and electrolytes in addition to mucus, to washout or dilute irritating factors. This causes rapid movement of feces towards anus resulting into diarrhea.
It is believed that extreme parasympathetic stimulation, caused by emotional disturbances, leads to Irritable bowel syndrome.
The passage of chyme from illeum into the cecum is regulated by ileo-cecal sphincter, which remains partially closed. Immediately after a meal, a gastro-ileal reflex intensifies peristalsis in the ileum occur which forces chyme into cecum. Pressure and chemical irritation of food relax sphincter and also excites peristalsis.
Absorption
Small intestine: The total quantity of fluid that must be absorbed each day by the intestine is equal to the ingested fluid plus fluid in various gastrointestinal secretions. Small intestine has many folds and millions of small villi present on it which increase surface area of absorption. More than 90% absorption of carbohydrates, proteins, fats, electrolytes, vitamins and water take place in upper portion of small intestine. Hepatic portal vein receives these nutrients from gastrointestinal tract. These nutrients are carried into liver sinusoids where these are taken up by hepatocytes for storage. Whenever needed they are secreted back into blood.
Large intestine: Chyme remains in the large intestine for about 3 to10 hours. Large intestine absorbs about 10% of water, out of total absorbed water. It also absorbs ions and some vitamins.
Chyme become solid and semisolid because of water absorption which is now called feces. Poor motility causes greater absorption of water leading to constipation.
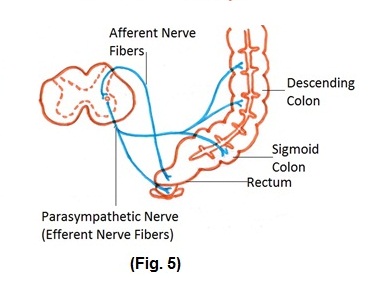
Defecation: Mass peristaltic movements push fecal material from the sigmoid colon into rectum. It results in distension of rectal wall stimulating stretch receptors which initiate defecation. (Fig. 5)
Liver and Pancreas
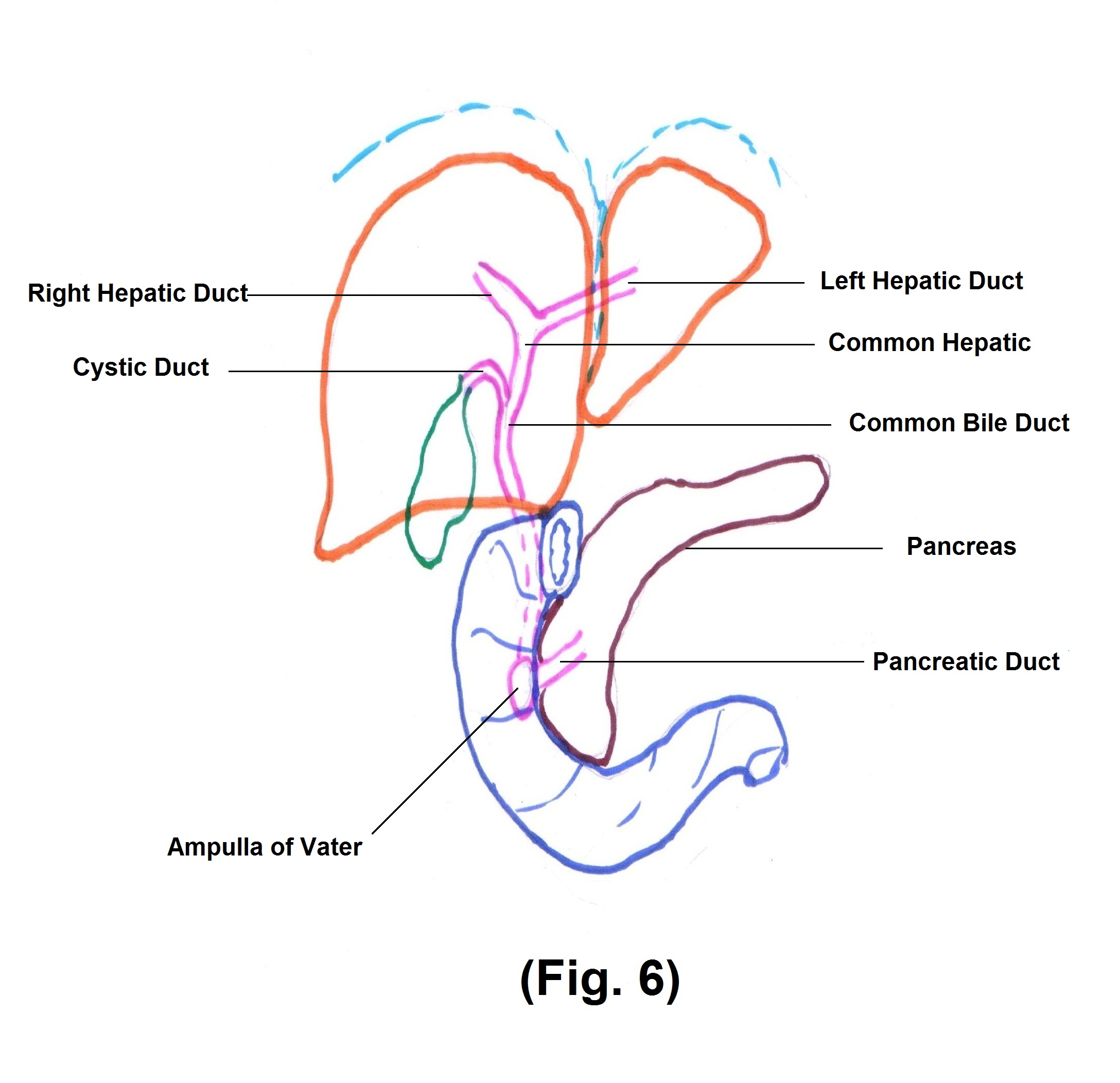
Liver and Pancreas are two important glands associated with digestion and metabolism. (Fig. 6).
Liver
The liver is a very large gland in the body. It occupies most of the right hypochondrium and small part of epigastric region in the abdomen. The gallbladder is a sac like structure situated in a depression of the liver. The gallbladder stores and concentrates the bile produced by hepatocytes.
Hepatocytes are the main functional cells of the liver. Bile produced by hepatocytes gets collected in small bile ducts. The ducts unite and form right and left hepatic ducts from right and left lobe of the liver. Common hepatic duct is formed by the union of right and left hepatic ducts. Common hepatic duct joins cystic duct from gallbladder to form common bile duct. Common bile duct joins the pancreatic duct to pour its contents into the duodenum.
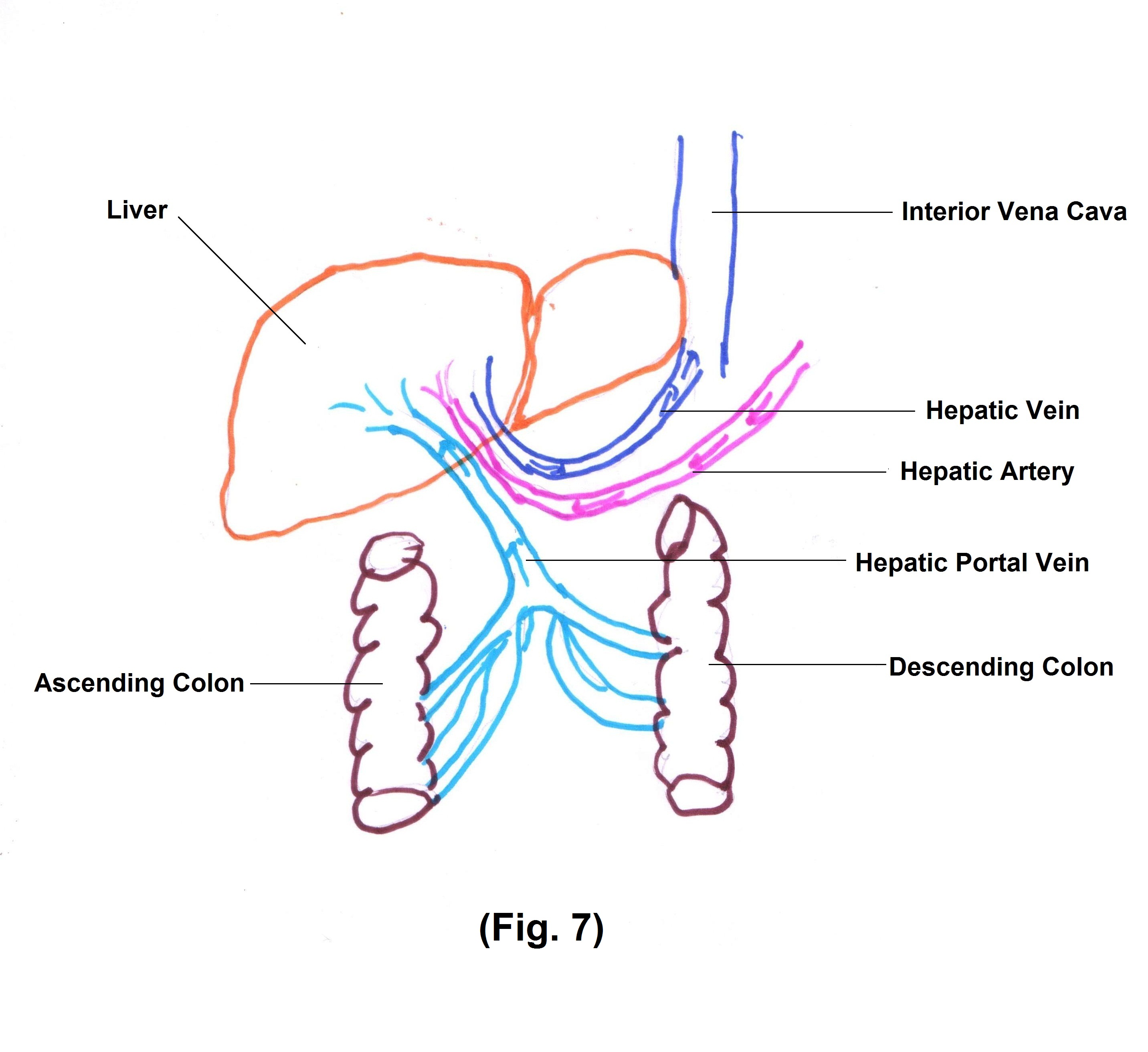
Blood supply to the liver is important. Liver receives (1) Oxygenated blood from hepatic artery (2) Deoxygenated blood through portal vein. Hepatic portal vein receives blood from capillaries of gastrointestinal organs and spleen and delivers it to liver sinusoids. Sinusoids are highly permeable blood capillaries receiving oxygenated blood from branches of hepatic artery and nutrient rich deoxygenated blood from branches of portal vein. Hepatic acinus is the smallest functional unit of liver where branches of hepatic artery, vein and bile ducts are converged. It is a transit zone, through which hepatocytes absorbs and store the nutrients and release toxic products to be drained out through hepatic vein, ultimately joining inferior vena cava. (Fig. 7)
Functions of liver:
- Liver is a principle organ in metabolic process. It participates in carbohydrate, lipid and protein metabolism.
- It detoxifies toxic substances. Liver participate in phagocytosis through Kupffer cells which is a part of reticuloendothelial system.
- Most of the drugs and few hormones like thyroid and steroid hormones are processed through liver.
- Liver absorbs bilirubin, which is a product of red blood cells degradation.
Bilirubin enters small intestine with bile and is excreted through faeces.
- Liver synthesize bile salts, used for lipid absorption and its further processing.
- It stores vitamins like A, B12, D etc.
Pancreas
Pancreas is a retroperitoneal gland lying in abdomen posterior to stomach. The pancreas contains glandular epithelial cells (about 99%) which are exocrine cells. The remaining 1% is pancreatic islets, which are endocrine in nature, secreting hormones – glucagon, insulin, somatostatin and pancreatic polypeptide.
Pancreatic juices secreted by exocrine cells are carried through small ducts ultimately forming pancreatic ducts. Pancreatic duct joins common bile duct from the liver and gallbladder to enter into the duodenum at a point called ampulla of vater. There is a sphincter at this site, called sphincter of oddi.
Pancreatic juice contains many enzymes participating in digestion.
