Urinary System
The urinary system can aptly be called as the filtration plant of our body, filtering blood plasma and excreting waste material along with urine.
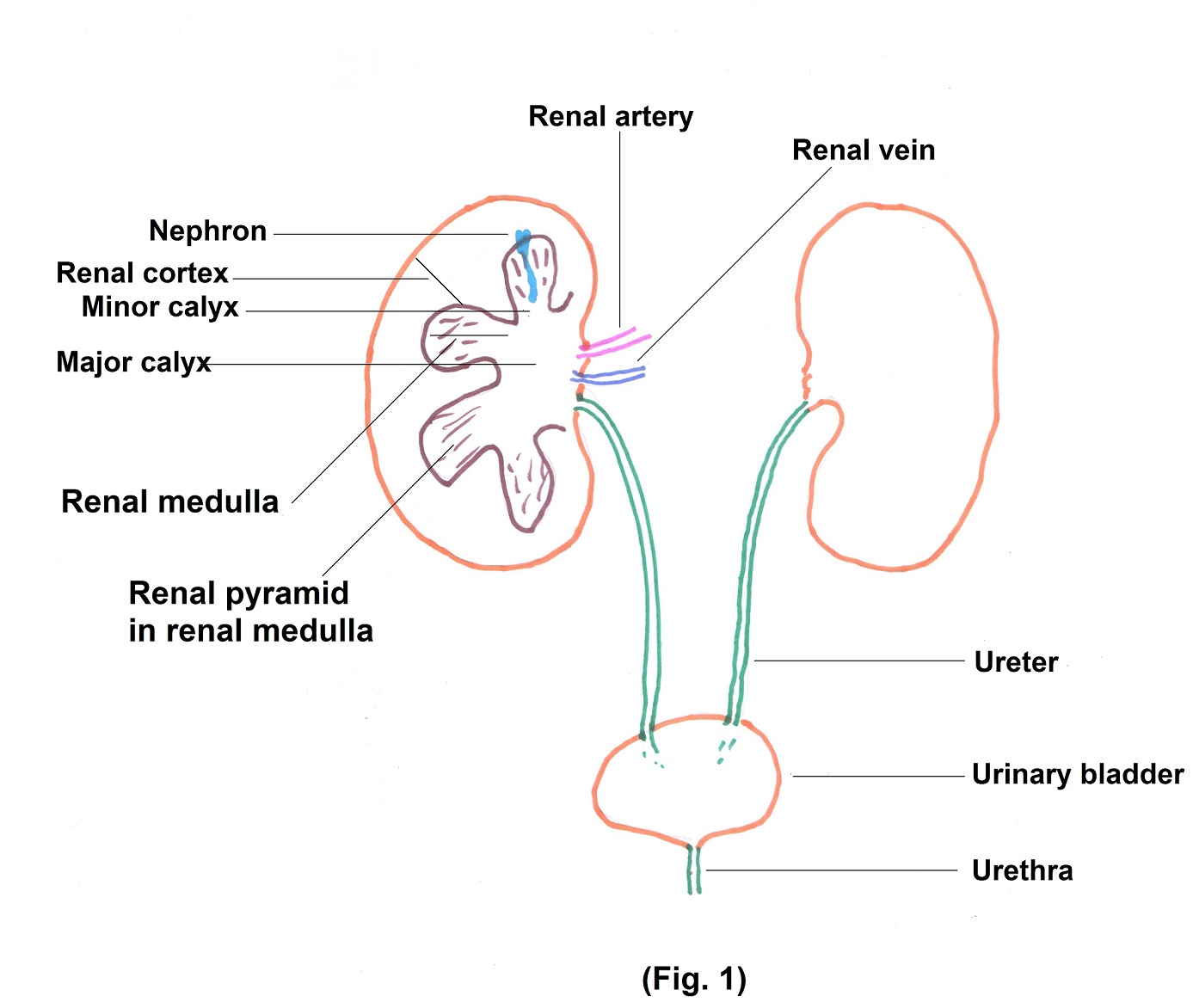
It consists of 2 bean shaped kidneys, lying on either side of the posterior wall of abdomen behind the peritoneum. The kidney is surrounded by renal capsule for protection. Inside, 2 distinct portions can be identified, renal cortex and renal medulla. The renal medulla consists of cone shaped structures called renal pyramids.
The renal cortex and pyramids together constitute parenchyma, the functioning part of the kidney. In the parenchyma, there are about 1 million microscopic structures called nephrons. Filtrate formed in the nephron, is drained in minor and major calyces through papillary ducts. Calyces are cup like structures which join each other to form renal pelvis. From renal pelvis, urine is drained into ureter and then into urinary bladder. From urinary bladder arises the urethra to excrete urine out of the body. (Fig.1).
Each kidney contains about 1 million nephrons which act as filters. We will study in brief, the structural and functional aspects of nephron. (Fig. 2)
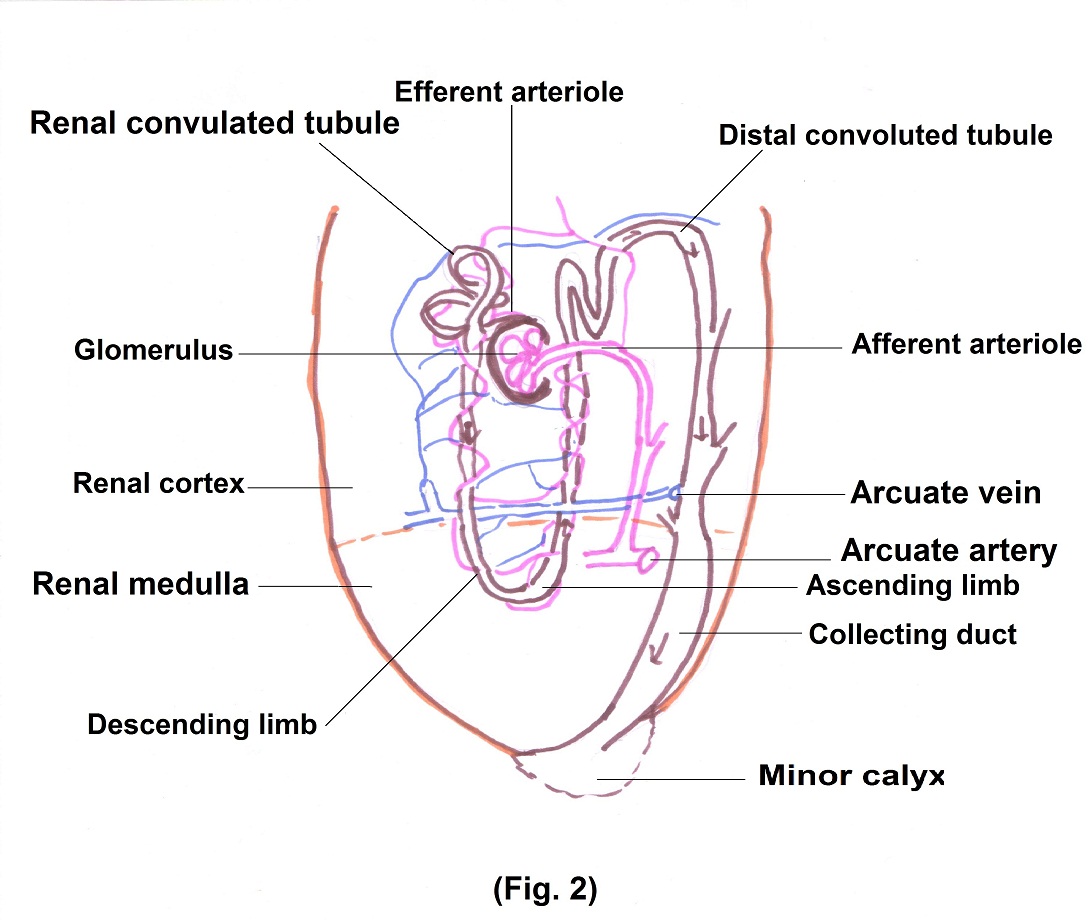
The blood reaches the kidney through the renal artery, which undergoes further branching to supply each nephron. The terminal branches further divide to form a ball shaped capillary network, called as glomerulus. The glomerulus is covered by a double layered membrane, called as glomerular capsule.
The space between the two layers is the glomerular space. It is here that the filtration occurs, and several factors are responsible for it.
- The capillary membrane has pores on it called as fenestrations which allow free flow of water and all solutes. However, it does not allow the passage of blood cells due to their large size.
- The membrane of the capsule has hollow passages called slits, which allow the passage of water, ions and all the nutrients. However, due to negative charges it does not allow the large negatively charged plasma proteins to pass through it.
- Other factors which play a role in filtration are hydrostatic pressure of blood and colloidal osmotic pressure.
Hydrostatic pressure is the pressure of blood against the wall of blood vessel. Colloid Osmotic pressure is the pressure exerted by proteins in blood which tend to pull water in the circulatory system.
The glomerular space continues into the tubule of nephron which has 3 parts.
- Proximal convoluted tubule (PCT)
- Loop of Henle with descending and ascending limbs.
- Distal convoluted tubule (DCT).
From glomerular space, the filtrate enters the PCT where major reabsorption of most of the water, electrolytes, small proteins and nutrients like vitamins and glucose occur. Secretion of hydrogen and ammonium ions, urea and creatinine occur here.
From PCT the filtrate enters loop of Henle. Further reabsorption of water and electrolytes occur here and urea is secreted in urine. Then filtrate enters into DCT, wherein further reabsorption of water and electrolytes occurs. Hydrogen ions and excess of potassium ions are excreted here.Distal convoluted tubules drain the urine into collecting ducts, from where it is carried into the ureter
Regulation of the process of filtration and reabsorption
It is regulated by various hormones. The most important is anti diuretic hormone (ADH). Normally, it is released by the posterior pituitary and it acts on the distal part of DCT and collecting duct by increasing its water permeability. When the concentration of water in the blood decreases or blood volume itself decreases posterior pituitary releases more ADH, which helps in water reabsorption back to the blood.
The second hormone is Angiotensin II. When blood pressure decreases, it stimulates cells in the renal arterioles to secrete the enzyme renin, which helps in the formation of Angiotensin II by hepatocytes. Angiotensin II stimulates the adrenal cortex to secrete the hormone aldosterone. Angiotensin II is a vasoconstrictor and Aldosterone helps in reabsorbing water from collecting ducts. Together, it leads to increase in blood pressure.
Other hormone is atrial natriuretic peptide(ANP). When blood volume increases with concomitant rise of blood pressure, increased level of this peptide inhibits the reabsorption of Na and H2O by the renal tubules. This in turn, increases urinary excretion, which helps return of blood volume back to normal.
Parathyroid hormone is an important calcium regulating hormone in the body. Its principle action in the kidney is to increase tubular reabsorption of calcium, especially in the distal tubule.
Autoregulation of Glomerular Filtration Rate (GFR) and renal blood flow:
Precise control of renal excretion of water and solutes is achieved by relative constancy of GFR and renal blood flow. This is termed as autoregulation.
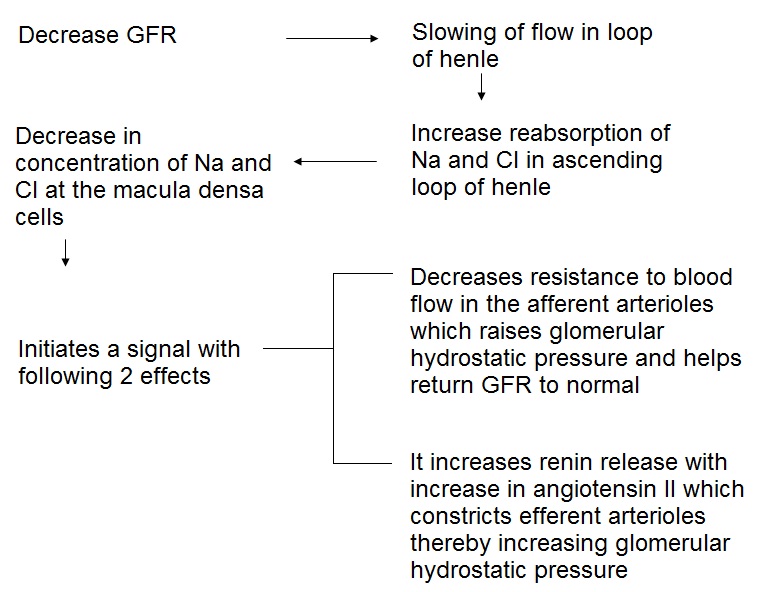
Macula densa is a specialised group of epithelial cells in the distal tubules that comes in close contact with the afferent and efferent arterioles. Decrease in GFR leads to following chain of events.
Urinary Excretion
From renal pelvis urine passes into the bladder through 2 ureters, one on each side. It is discharged from the bladder through urethra. (Fig.1)
Ureters
Ureters are 25-30 cm long narrow tubes varying in diameter from 1mm to 10mm as they traverse down from renal pelvis to urinary bladder. Peristaltic contraction of muscular walls of ureter puts the urine towards bladder. When urinary bladder is full, the backflow of urine into the ureter is prevented as the oblique opening of ureter into bladder gets compressed. If this mechanism does not operate properly urinary infection can travel to kidney.
Urinary bladder:
It is a hollow muscular sac in the pelvic cavity posterior to public symphysis. In males, it is anterior to rectum. In females, it is anterior to vagina but inferior to uterus. Urinary bladder capacity is about 700-800 ml. In the bladder, there are 2 ureteral and one urethral opening called internal urethral orifice. The sphincter at internal urethral orifice is involuntary. Little further there is external urethral sphincter which is under voluntary control. (Fig.1)
When 300 to 400 ml urine collects in the bladder one gets a sensation of fullness and desire to urinate. Concomitantly, stretch receptors in the walls of bladders send nerve impulses to micturition centre in the sacral region (S2, S3) of spinal cord. Following that from micturition centre parasympathetic impulses travel to urinary bladder wall and internal urethral sphincter. Co-ordinated action of various muscles of bladder results into act of micturition. Micturition reflex has learned control by which cerebral cortex can initiate or delay micturition.
Urethra
In males, urethra passes through the prostate, through the muscles of perineum and ultimately through penis, a distance of about 20 cm. In males, semen is also discharged out through urethra. In females, it is short, about 4 cm in length and its external urethral orifice is located between clitoris and vaginal opening.
