Liver, Gall bladder and Pancreas
We will try to study most common disorders of liver and gall bladder, starting with common presentations and the manner, a clinician thinks in resolving the problem.
A patient presents with fever with other constitutional symptoms like body ache, lethargy, loss of appetite, maybe vomiting once or twice. He is treated symptomatically. After 2 – 3 days fever may disappear, loss of appetite, vomiting may continue, he also complains of abdominal discomfort and yellow urine. His liver may be palpable, tender and soft.
Occasionally there may not be fever, but he will come only for loss of appetite, yellow urine, lethargy etc.
One can suspect viral hepatitis and liver functions tests are advisable.
Liver function tests
- Bilirubin – Bilirubin is the principle bile pigment, a constituent of bile stored in hepatocytes. Bilirubin level reflects degree of liver damage. Clinically evident jaundice appears when bilirubin level exceeds 3mg.
- Alkaline aminotransferase (ALT) and aspirate aminotransferase (AST) are located in the cytoplasm of hepatocytes. Expression of ALT outside the liver is low. Therefore, this enzyme is considered more specific for hepatocellular damage.
- Alkaline phosphatase (ALP) and gamma glutamyl / transferase (GGT) – ALP consists of several enzymes. The main site of its production is liver, G.I.tract etc. In the liver these are located in cell membranes of hepatic sinusoids and biliary canaliculi. Therefore, its rise indicates intra or extra hepatic biliary obstruction.
GGT is produced by hepatocytes by epithelium lining small bile duct.
Large increase in ALP and GGT activity favours biliary obstruction. Isolated elevation of GTT is common.
It should be noted that transient mild abnormalities of LFT are not clinically significant. Persistent abnormality indicates liver disease especially alcoholic and non-alcoholic fatty liver disease.
Jaundice
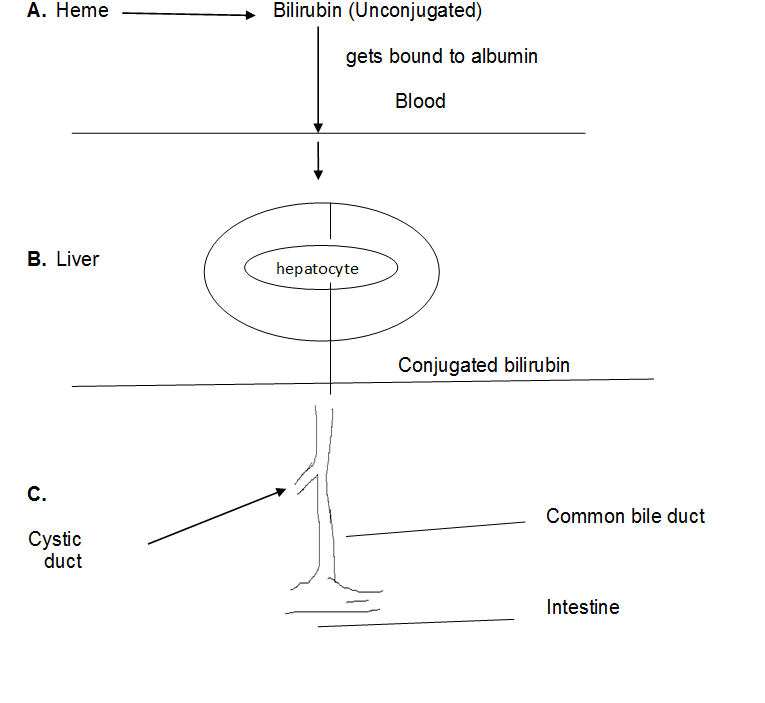
After doing LFT in a patient of jaundice (yellow sclera, skin, increased bilirubin and alteration in ALT, AST etc.) one has to decide the basic cause and the type of Jaundice. Let us review bilirubin metabolism.
Hepatocytes secretes bile which consists of water, bile salts, bile pigments etc. Principle bile pigment is bilirubin. This is derived from heme which is a product of aged RBC.
Secreted bile reaches intestine through bile canaliculi, bile duct, hepatic duct which joins cystic duct from gall bladder forming common bile duct which opens into intestine. A small part of bile is used for digesting the fatty substances while rest is reabsorbed and stored into the gall bladder.
Bilirubin is converted to stercobilin in intestine which gives brown colour of faeces.
Bilirubin is in unconjugated form before entering into liver. It is insoluble in water, gets bound to albumin and enters liver. In hepatocytes conjugated bilirubin is formed which is soluble in water.
A. Pre-hepatic Jaundice –
If haemolysis is increased due to any reason, e.g. Haemolytic anaemia, bilirubin is raised, predominantly unconjugated bilirubin.
B. Hepatocellular Jaundice –
This occur due to parenchymal liver disease, most common being viral hepatitis. It is associated with rise in both, unconjugated and conjugated bilirubin.
C. Obstructive (Cholestatic) Jaundice –
It results due to obstruction of bile flow. The cause may be intrahepatic liver biliary cirrhosis, cholangitis etc. or extrahepatic due to carcinoma. Clinically along with jaundice, pale stool, dark urine, pruritus (due to deposition of bile salts) may be noted. Cholangitis may be associated with fever, pain due to underlying gall stones.
Obstructive jaundice may need surgical intervention.
Viral hepatitis
The most common cause of hepatitis is infection by a group of viruses.
- Hepatitis A virus: It is self-limited disease and rarely causes severe hepatitis. It does not result into chronic form or carrier state. Clinically it is mild, asymptomatic or may have nonspecific symptoms like fever, fatigue etc. Specific IgM antibody against HAV appears in the blood and is a reliable manner of acute infection.
2. Hepatitis B virus (HBV): It can produce
i. Acute disease clearing out completely
ii. Non-progressive chronic hepatitis
iii. Progressive hepatitis leading to cirrhosis
iv. Occasionally severe hepatitis with marked liver necrosis
v. Carrier state
The infection can occur in perinatal period during childbirth. Later on, it can occur through minor cuts, breaks in skin or mucous membranes, during transfusion etc.
Although the disease runs a mild course, various directions it can proceed should be kept in mind.
IgM anti HBs can be detected early along with elevated serum amino transferase level.
Hepatocyte damage is believed to occur because of damage to virus infected cells by CD8 + Cytotoxic T cell. Thus, immune response to virus is important in protection.
3. Hepatitis C virus: In contrast to HBV, progression to chronic disease is common in HCV, leading to cirrhosis. Most of the time the infection is blood borne.
Acute infection can be missed as it is asymptomatic. In chronic HCV infection episodic elevation in amino transferase is common. The diagnosis can be made with HCVRNA testing.
4. Hepatitis D virus: Infection occurs along with HBV. If it occurs as superimposed infection in chronic HBV carrier, acute severe hepatitis can occur.
5. Hepatitis E virus: It is self-limiting mild infection.
Liver Cirrhosis
Liver cirrhosis is a histologic diagnosis and is characterised by hepatic fibrosis and nodule formation.
Chronic viral hepatitis and alcoholic hepatitis are the common causes leading to cirrhosis.
The presentation is variable.
- Asymptomatic patient and incidentally on USG finding, one can think of cirrhosis.
- Isolated hepatomegaly, Splenomegaly
- Signs of portal hypertension.
Liver is palpable, often found, nontender with irregular margins. Spider telangiectasis (a central arteriole from which small vessels radiate) may be visible above nipples.
Portal hypertension results due to sinusoidal blockage due to surrounding fibrosis. Splenomegaly, caput medusae (collateral vessels radiating from umbilical region) can occur. Variceal bleeding especially from oesophagus can occur because of oesophageal varices. Similarly bleeding from haemorrhoids due to rectal varices. The diagnosis can be made on clinical ground. Endoscopic examination is necessary to decide the extent of varices. Ascites may occur as the disease advances.
Gallbladder and Biliary disease
Gall stone and the related disorders arising there from are commonly seen in practice. In most of the cases, cholesterol and pigment stones are formed.
Various factors lead to stone formation. For example, excess production of cholesterol in bile is noticed in old age, obese people, and in females. Impaired gallbladder emptying may occur in pregnancy, fasting etc.
Clinically majority of patients with gall stones are asymptomatic. Symptomatically gall stones are manifested either as biliary colic or cholecystitis.
If a gallstone gets impacted in cystic duct severe pain occurs either in epigastrium or right upper quadrant which may radiate to back or tip of the right scapula. It occurs suddenly and may last for 2 to 3 hours. Cholecystitis or pancreatitis can be suspected. Biliary colic is to be differentiated from myocardial infarction, oesophagitis etc.
The gall bladder stones (Cholecystolithiasis) may descend down to common bile duct (Choledocholithiasis) and cause biliary colic.
Occasionally impacted gall stone cause obstructive jaundice. The stone descending into common bile duct can cause cholangitis or acute pancreatitis. USG is essential for diagnosis of gallstones. CT is a better choice to detect complications of gallstones.
Acute Cholecystitis
It is almost always associated with obstruction of gallbladder neck or cystic duct by a gallstone. It leads to inflammation. Symptomatically it resembles biliary colic. In cholecystitis pain is generally more severe, prolonged and may be with fever and leucocytosis. Rigidity in rt. hypochondrium worse on inspiration (Murphy’s sign) is typical of cholecystitis.
Minor elevation in transaminase and amylase are common. Marked rise in amylase, more than 1000 U/L points to pancreatitis.
Acute cholangitis can occur due to bacterial infection of bile duct in patients with biliary problem. Jaundice, abdominal pain is the presenting symptoms.
Pancreas
A patient with severe pain constant upper abdominal pain radiating to the back with nausea and vomiting, pancreatitis should be ruled out.
Acute pancreatitis results from premature activation of zymogen granules, releasing proteases which digest the pancreas and affect surrounding structures like common bile duct, duodenum, splenic vein etc. The severity of the disease depends on released proteolytic enzymes and antiproteolytic factors. common causes of acute pancreatitis are gallstones, alcohol and many times it may be idiopathic.
If not treated properly it may lead to complications and sometimes fatal outcome.
The diagnosis is based on finding raised serum amylase or lipase concentration and USG or CT evidence of pancreatic swelling.
Chronic pancreatitis
It is a chronic inflammatory disease. A cycle of inflammation and fibrosis leads to chronic pancreatitis. It occurs in alcoholics but can be found in non-alcoholics also.
Intermittent abdominal pain, weight loss due to malnutrition is common.
